AUSTIN, Texas — Essential workers, low-income earners and people living in dense environments faced higher risk of COVID-19 infection and hospitalization, even amid COVID-19 shelter-in-place policies, according to a new study from public policy researchers at The University of Texas at Austin. The study, appearing in Plos One, showed that these individuals faced more challenges to comply with pandemic lockdowns.
Researchers at UT Austin’s LBJ School of Public Affairs also created a policy modeling framework to help explore critical trade-offs between effectiveness and equity with the hope that policymakers can better design policies with society’s most vulnerable in mind.
“We have a limited ability to understand and anticipate the potential impacts of policies on local communities and across socio-demographics,” said Vivek Shastry, a graduate research assistant in the LBJ School and lead author of the study. “Though it’s impossible to precisely predict the trajectory of unfolding complex events, using tools like this can help decision makers put in place additional welfare measures to protect the most vulnerable populations.”
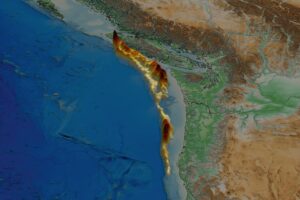
When a crisis arises, it presents an opportunity for a timely policy response. But when things unfold rapidly, much can get in the way, including failure to consider alternative options and lack of research. Using a modeling framework, researchers can incorporate several of these challenges to model real-world responses to policy. In this case, researchers modeled real-world responses to shelter-in-place policies during a one-month period in Austin, Texas.
The simulated policy scenarios show a trade-off between effectiveness and equity in the distributional impact of shelter-in-place timing across different income groups. For example, in the early timing scenario, hospitalizations among individuals in the lowest income group were disproportionately high in the second peak – close to 45% of those who were hospitalized belonged to the lowest income group, who only composed 22% of the population.
“This suggests that, despite lower prevalence of hospitalization in the system, the burden of hospitalization that remained was disproportionately borne by those in the lowest income group,” said Varun Rai, a professor in the LBJ School of Public Affairs who co-authored the study. “For lower income and other vulnerable groups who make up a higher proportion of the essential workforce, the social context of their work in high-frequency interaction work environments such as restaurants or grocery stores, and the inability to comply with social distancing guidelines puts them at a higher risk of infection and hospitalization.”
The researchers said that although it is impossible to precisely predict the trajectory of rapidly unfolding complex events, using tools such as this can provide insight into the higher-level trends that can help decision makers put in place additional welfare measures to protect the most vulnerable populations.
The model also provided insights on how timing affects policy. Researchers use the model to show that even in a scenario where the shelter-in-place policy had been implemented a couple of weeks earlier than it was, although it would have been successful in reducing the overall hospitalizations, those in the lowest income group still would have had a disproportionately higher share of the hospitalization burden.

![TransportationWorker_Credit_RobinsonGreigUnsplash[58] copy](https://news.utexas.edu/wp-content/uploads/2022/03/TransportationWorker_Credit_RobinsonGreigUnsplash58-copy-600x400-c-default.jpg)