Decades of scientific progress — including breakthroughs in imaging, targeted therapies and early detection — have modernized breast cancer treatment. Now, researchers at The University of Texas at Austin are studying new solutions to detect and treat even the most aggressive forms of breast cancer using data, cutting-edge technologies and collaboration across disciplines.
These innovations are only the beginning of what UT Austin researchers and physicians will accomplish together with an integrated, academic health system. The emerging UT Medical Center — anchored by Dell Medical School and strengthened by a historic partnership with MD Anderson, the nation’s #1 cancer center — will make it possible for researchers and clinicians to collaborate in even more ways to accelerate breakthroughs in research and patient care.
Powerful Proteins
Certain types of breast cancer, including inflammatory breast cancer (IBC) and triple-negative breast cancer (TNBC), remain incredibly difficult to treat. Although rare, these two very aggressive forms of the disease account for nearly half of breast cancer deaths, largely because they respond poorly to standard treatments and often develop treatment resistance over time.
UT and Houston-based MD Anderson Cancer Center have teamed up to change that. Using samples provided by MD Anderson, one of the country’s leading cancer centers, researchers across UT’s Cockrell School of Engineering, College of Natural Sciences and Center for Biomedical Research Support will identify areas of weakness in IBC and TNBC cancer cells and develop new protein-based therapeutics designed to attack those vulnerable areas.
From Simulation to Solution

What if a computer model could predict how your body will respond to treatment before it even begins? That’s the goal of Michael Sacks, biomedical engineering professor and director of the Willerson Center for Cardiovascular Modeling and Simulation. He and his team of multidisciplinary researchers are building the most accurate computer model of the breast to date.
A global authority on cardiovascular modeling and simulation, Sacks has created simulations of the human heart that examine its functionality at the cellular, tissue and organ levels.
Sack’s breast model, which is being funded through a grant from the National Institutes of Health, will reflect the way breast tissues behave and move in real life — a feat that has never been successfully done before in modeling. This highly advanced model will help with everything from locating tumors to training surgeons and designing post-mastectomy recovery clothes. It can also lead to more personalized patient care.
Turning Mutation Into Medicine

In the microscopic war between healthy and cancerous cells, one enzyme is playing both sides — and UT researchers may have just figured out how to tip the balance. The enzyme in question, APOBEC3B, is typically used by cells to fight viruses. However, it can mistakenly attack the cell’s own DNA at vulnerable structures called R-loops, triggering mutations that help cancer cells evolve and resist treatment. About 20% of breast cancer tumors (and 50% of other cancerous tumors) produce an excess of APOBEC3B, which is related to worse patient outcomes.
Molecular biosciences professor Kyle Miller and his team are investigating a hypothesis that increasing the number of R-loops in cancer cells with high levels of APOBEC3B could cause so many mutations that it overwhelms the cancer cells, killing them. This concept could lead to a new approach in cancer therapy: overwhelming the cancerous cells from the inside out. The Food and Drug Administration has already approved drugs that increase R-loops, which could help move this approach toward clinical application more quickly.
Breaking Down Barriers
On average, 80% of women in the U.S. ages 50-74 have had a mammogram during the past two years. But that number drops considerably for those without medical insurance. Since 2021, Dell Medical School, with support from a variety of community partners, has provided free, mobile mammograms through its cancer screening and early detection program, serving patients in Central Texas who experience socioeconomic barriers to care. Without such intervention, these individuals are more likely to be diagnosed with breast cancer at later stages, face more complications that reduce their quality of life, and experience higher mortality rates. Thanks to a $2 million grant from the Cancer Prevention & Research Institute of Texas, Dell Med’s program is expanding services to more counties, increasing its mobile mammography screenings, and adding 24 new fixed testing sites and 17 new clinic referral sites, substantially increasing the number of women who can benefit.
When Algorithms Meet Oncology

As technology advances, so do our ways to combat complex illnesses, including cancer. With the help of the Texas Advanced Computing Center (TACC), home of the fastest academic supercomputer in the world, researchers at the Oden Institute for Computational Engineering and Sciences are using advanced computing to innovate breast cancer diagnosis and treatment.
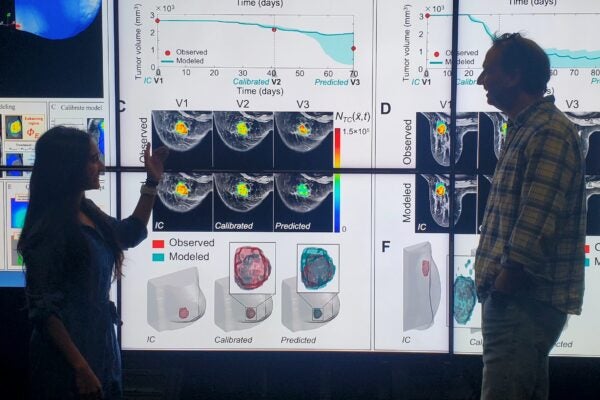
Using patient MRI scans, Thomas Yankeelov, biomedical engineering professor and director of the Center for Computational Oncology (CCO), and his team developed biology-based mathematical models to predict how triple-negative breast cancer tumors will respond to treatment. Using patient MRI scans from the beginning of the treatment and at the three-week mark, the model will forecast the tumor’s changes after nine weeks. In the future, Yankeelov hopes this “digital twin” can also be used in trials for a variety of treatments, including chemotherapy, hormone therapy and immunotherapy, to identify those most likely to work, helping doctors create a highly individualized treatment plan for each patient.
Meanwhile, CCO research scientist Ernesto Lima created mathematical models to optimize the treatment for HER2-positive breast cancer, an aggressive and fast-growing form of the disease. Using high-tech simulations, Lima and his team found the ideal order and timing for the delivery of two powerful drugs, shrinking tumors by 45% without increasing the dosage, leading to fewer side effects for the patient. They even figured out a way to reduce one of the medication’s doses while achieving the same shrinkage. The team’s next step is to test their treatment plan in real-life settings. If the results are the same, it could lead to safer, more effective treatments.
Additionally, a team from the Oden Institute and MD Anderson has used natural language processing to make mammograms more effective. Their data pipeline reads radiology reports and creates a visual map of the breast, pinpointing areas of concern. The tool can also line up current and previous mammograms side by side to help doctors spot and track changes over time.
The effort is part of a new partnership between UT and MD Anderson supporting and accelerating groundbreaking research aimed at improving cancer prevention, diagnosis, treatment and survival.
Redesigning Reconstruction

For many women, breast reconstruction is a key phase in recovery, but this complex surgery is not always straightforward. It can often be an arduous process involving multiple surgeries, overwhelming decisions and outcomes that depend largely on the surgeon’s experience.
Biomedical engineering professor Mia Markey is leading a multi-institutional research team in the creation of custom 3D breast molds for patients undergoing reconstructive surgery. Backed by a grant from the NIH, the team will develop a clinical algorithm to help surgeons design personalized molds for shaping the reconstructed breast tissue during surgery. The customization of the molds will allow patients to create a breast that suits their post-mastectomy body rather than re-creating their preoperative appearance, which can help improve their mental health and aid them in adjusting to life after cancer. They should also reduce the cost of reconstruction and the number of follow-up procedures.
This isn’t Markey’s first foray into the world of breast reconstruction. She previously played a key role in developing computer models of the breast to help surgeons improve the precision of reconstruction.
World-Class Data, UT Stewardship

Thanks to a generous donation from cancer researchers Jim and Mitzie Wittliff, UT now holds one of the most extensive breast cancer data collections in the world. Through their work at the University of Louisville, the Wittliffs spent decades collecting more than 5,000 samples from breast, ovarian, endometrial and colon cancers. Among those samples is some of the most detailed and carefully measured data on breast cancer biomarkers, including measurements from the tests that became the “gold standard” doctors use to determine what type of breast cancer a patient has.
But it’s not just the samples that make this donation special. It’s the wealth of information that comes with it. Many of the samples come with accompanying data detailing everything from tumor type to treatment history and patient demographics, giving scientists a rare look at how cancer behaves and responds to treatment over time. It also allows researchers to look for patterns, which can lead to better tests, treatments and ways to predict the risk of recurrence.
The Witliff samples are now stored at Dell Medical School, and accompanying data is housed and managed at TACC. UT experts plan to analyze the information and eventually share it with researchers around the world.