At Dell Medical School, the Neonatal-Perinatal Medicine Fellowship is preparing the next generation of physician leaders to advance care for the smallest and most vulnerable patients. In partnership with Ascension Seton and Dell Children’s Medical Center, fellows gain hands-on experience in a high-acuity environment that blends cutting-edge technology, compassionate family-centered care and a commitment to innovation.
As the University builds an integrated academic medical center anchored by Dell Med in the coming years, academic medicine is already having a measurable effect on local care: U.S. News & World Report’s 2025-2026 Best Children’s Hospitals lists recognized Dell Children’s Medical Center as a top hospital for neonatology care, and its affiliated Texas Center for Pediatric and Congenital Heart Disease is now ranked No. 10 in the nation, previously unranked until 2023. Having high-acuity neonatal care close to home means Austin families no longer need to travel far distances for specialized treatment, allowing them to stay connected to their support networks during critical times.
The fellowship program also offers comprehensive point-of-care ultrasound (POCUS) training, a field that has expanded significantly in neonatal care over the past decade. Under the leadership of Alan Groves, M.D., all fellows acquire essential POCUS skills (vascular access, assessment of pleural and pericardial effusions and cardiac evaluation) and advanced training opportunities in diagnostic and procedural POCUS and targeted neonatal echocardiography (TNE). This makes it possible for clinicians to deliver more precise, individualized care with less invasive testing — leading to fewer physical disturbances to babies in care.
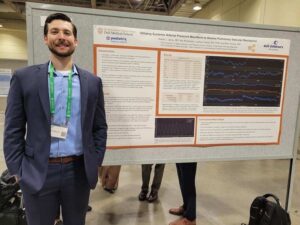
As one of the first physicians to complete Dell Med’s Neonatal-Perinatal Medicine Fellowship, Dr. Jesse Janes embodies that spirit of discovery and growth. Drawn to the program’s pioneering energy and culture of collaboration, Janes helped shape the fellowship during its inaugural years. Now, Janes is pursuing additional training in neonatal hemodynamics through the University of Iowa and serving as an assistant professor in Dell Med’s Department of Pediatrics, where he’ll work to establish a new neonatal hemodynamics program.
Read on to learn more about Janes and his passion for advancing neonatal care through education and innovation.
1. You were part of Dell Med’s inaugural fellowship class in Neonatal-Perinatal Medicine. What drew you to be part of a brand-new program?

I love being a part of new things and seeing them grow. It’s one of the reasons I became a neonatologist! When I met with the fellowship program leadership on my interview day and heard just how much thought and care went into crafting this training program, I was instantly drawn in. There was an electricity among the faculty who were seeing a longstanding dream coming to fruition. It felt like I found an opportunity to take part in the start of something special.
I’m happy to say my expectations were completely fulfilled by my experience in the fellowship. The process of helping to shape a program from its infancy was and is an incredibly rewarding aspect of my time at Dell Med. In addition to learning the practice of neonatology, I was able to take part in trying out new ways of learning, improving upon parts that could be done differently, and refining the aspects of training already going well. We were able to do this without the burden of working against “the way we’ve always done things.” In fact, I’ve found our unit’s culture of support for one another in growth and well-being provides the perfect setting to explore new ways of innovating the fellowship experience.
2. After completing the fellowship, you’ve continued on with Dell Med as an assistant professor in the Department of Pediatrics. What does it mean to you to be part of the faculty, and what do you hope to pass on to the next generation of fellows?
I am very excited to continue working in our NICUs and with Dr. Alan Groves, who has already established a successful neonatal POCUS program at our institution. His expertise in both POCUS and neonatal hemodynamics was a tremendous resource and source of mentorship during my fellowship and remains as I pursue further training while continuing to practice as an attending physician. With the completion of the hemodynamics fellowship, I hope to contribute to a critical mass of skill and training at our institution to establish a hemodynamics service to continue advancing the ways we serve our patients.
With this in mind, I look forward to sharing my passion and knowledge with the current NICU fellows. Throughout my medical education and training, I’m fortunate to have benefited from numerous clinicians and professionals who have shared their interests and encouraged me to seek new experiences. Because of these relationships, I am a better neonatologist, researcher and advocate for my patients. I hope to pay it forward to the coming classes of trainees at our institution and help our trainees find their own passions. In this, I’m honored to join a group of neonatologists who have invested so much of their time into preparing my co-fellows and myself for a lifetime of caring for babies. I’m eager to share in their dedication to providing the best training to future generations of physicians.
3. You’re pursuing additional specialized training in neonatal hemodynamics at the University of Iowa. What advanced skills are you gaining that you’ll bring back to Austin?
I am thrilled to be accepted as an external fellow in the University of Iowa neonatal hemodynamics training program. This hybrid-style fellowship will allow me to learn the skills needed to establish a neonatal hemodynamics program here in Austin while continuing to practice here as a neonatologist during this training. I am grateful to my division chief, Dr. John Loyd, and my mentor, Dr. Alan Groves, who is a leader in the field of neonatal hemodynamics, for their support and guidance as I complete this fellowship.
During this training, I’ll learn from some of the world’s premier hemodynamicists about how to utilize an ultrasound technique called targeted neonatal echocardiography, or TNE, to give insight into a patient’s hemodynamic status. This thorough evaluation involves the capture of over a hundred images and the synthesis of dozens of measurements to develop an understanding of how well the chambers of the heart are functioning and how effectively blood is being pumped out to the body and returned back to the heart. In patients who are critically ill and receiving hemodynamic therapies, this data is especially important as their physiology can change rapidly, and TNE can allow us to monitor for these shifts. Right now, there are only a handful of NICUs in the country with neonatologists trained to perform this type of exam. My aim is to add our institution to this elite list.
4. How does understanding cardiac physiology and hemodynamics change the way you care for the tiniest, most vulnerable patients?
In our smallest, sub-500-gram babies who are born more than four months before their due date, finding the perfect balance in supporting every one of their organ systems is a task sometimes requiring minute-to-minute or second-to-second changes in care. When taking care of such fragile infants, it can be complicated to balance the need for investigation with the risks of obtaining that information. Even the physical stimulation of obtaining a blood sample or taking an X-ray can be destabilizing to an extremely premature infant.
In such cases where the margin of error is razor thin, the ability to use a radiation-free, delicately performed ultrasound to have a window into a baby’s physiology can provide critically important data when choosing the most appropriate way forward. TNE is a modality we are working on adding to our ever-expanding array of tools to care for our sickest and most vulnerable patients. Because no two babies are the same, especially the most extremely premature infants, we are adding more emphasis on providing each patient with the care that best fits their needs. With a personalized TNE evaluation of hemodynamics, we continue to move ever closer to an individualized model of care where every patient’s plan of care is made specifically for them.
5. As UT builds an integrated academic medical center, how does having a strong fellowship program translate to better care for Austin’s families and their babies?
The presence of inquiring minds in any unit benefits everyone involved, from patients to bedside staff to attendings. Learners, whether they are fellows, residents or students, are key members of the team. When they bring an attitude of curiosity into the unit, it keeps everyone sharp and accountable for having the most up-to-date information on current research, evidence for clinical care, and it pushes us to consider new ideas from fresh perspectives. With this, our patients benefit from our care being constantly honed and refined through the process of teaching, listening, learning and relearning that goes along with being a part of a training program. I firmly believe our babies are best taken care of by a team dedicated to training future clinicians.
6. Dell Children’s is being recognized as being among the nation’s best for neonatology by U.S. News & World Report. From your perspective, what makes the neonatology program special?
Our NICU’s recognition as one of the best in the country is a tremendous honor, but not one that comes as a surprise. I see it earned every day through the great effort and diligence put in by our whole team in caring for babies and their families. During my past few years at this institution, I came to understand that a big part of our ability to take care of our patients at such a high level comes from the commitment to taking care of one another. The NICU is an immensely emotional place full of great joys and deep sorrows, and our team is dedicated to supporting one another through those times and everything between. One result of this interconnection is the opportunity to really understand one another as people and as professionals. In doing this, we can find ways to engage each person’s unique strengths in our pursuit of excellence. It is this culture that drew me to the institution and made me want to stay as a member of the faculty.
7. What does it mean for Austin families that more high-acuity neonatal care is available close to home, rather than having to travel to other cities?
Taking care of our neighbors in Central Texas is a privilege and honor. Every day, we as a team strive to live up to the trust placed in us by our patients and their families. With our ever-expanding capabilities in the NICU, it is great to know families don’t need to travel hundreds of miles away from their friends, family and other support networks for their baby to receive the best care. Because even with all the support we can give, we know we can never fill the role of a trusted friend or loved one in holding our families through the difficulties that can come with having a baby in the NICU. In addition to this, the logistics of keeping up with jobs, childcare, grocery shopping, and every other aspect of life outside of the NICU continue on, and being close to home can help make a stressful situation just a little more manageable.