AUSTIN, Texas—In the future, doctors may be able to heal damaged tissue faster using a unique blend of biological and inorganic materials. These “biomaterials” are the next frontier in the field of tissue engineering, which involves growing tissues in the lab for research and grafting as well as stimulating the body into regenerating its own tissue more quickly.
Christine Schmidt, a 33 year-old assistant professor in the department of chemical engineering at The University of Texas at Austin, has developed a new biomaterial consisting of a plastic dotted with a sugar group, which can stimulate the body’s healing processes.
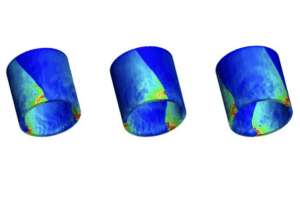
“The bottom line is to have a material that we can implant into the body that encourages nerves to repair themselves better, faster and over larger areas,” Schmidt said. “We implant the biomaterial as a conduit that basically patches the damaged nerve ends together — in a sense, like a tubular Band-Aid. The biomaterial is formed into a tube that would then be surgically implanted around the damaged nerve ends,” Schmidt explained.
The material has not yet been used on humans. However, tissue cells from rats can grow twice as quickly on this biomaterial in the laboratory than on plastics previously used, said Schmidt.
Her research is detailed in an article to be published in the April issue of the Journal of Biomedical Materials Research. Schmidt reported on her work at the annual meeting of the American Chemical Society in San Francisco on Wednesday (March 29).
Schmidt said the goal of this research is to repair peripheral nerve defects, such as injuries to nerves in the arms, legs and face that could result from trauma such as gunshot wounds or car accidents. Among many other applications, the research also could be of benefit in reconstructive surgery. While it does not directly apply to spinal cord injuries, it could provide insights to scientists working in that area.
The plastic and sugar mix gets its extra punch by combining the special properties of each ingredient. The sugar, naturally found in the body, can trigger certain cellular responses to make blood vessels form more quickly, while the plastic can conduct electricity that stimulates growth, Schmidt explained. Schmidt said this process is unique.
“To our knowledge, no one else is directly targeting blood vessel growth for nerve repair, and no one else is using an electrically conducting polymer (plastic) to stimulate the repair process,” Schmidt said.
She found that blood vessels, vital for supplying oxygen and nutrients to cells, grew in higher numbers and larger sizes on the new biomaterial than occurred on plastics used in previous research. Schmidt said, however, that the sugar dissolved too quickly to be as effective as researchers want it to be.
It would be more effective for promoting blood vessel growth if the sugar disappeared more gradually. Schmidt said as with “time-release pills for certain medicines, (it is) better to spread out the effect of the drug over a longer period of time.”
Schmidt said she hopes to overcome these problems by linking the sugar molecules together so they can’t dissolve as quickly. Certain other molecules can link the sugars by forming chemical bonds between them. New research currently in progress will examine the potential for developing a time-release system and explore other biological molecules that stimulate blood vessel growth.
Chemical engineering doctoral candidate Terry Hudson assisted Schmidt with the research, along with Joel Collier and James Camp. Collier is now a biomedical engineering doctoral candidate at Northwestern University, and Camp is a biomedical engineering doctoral candidate at MIT.
The research was funded by a National Science Foundation Early Career Development (CAREER) Award of $250,000 over five years, a University Cooperative Society Fellowship of $1000 in supplies and a one-year $65,000 grant from the Gillson Longenbaugh Foundation for biomedical research.
For more information, contact Becky Rische at the College of Engineering, (512) 471-7272. Dr Christine Schmidt can be reached at the American Chemical Society meeting press office at (415) 923-7510, returning to UT Austin on Friday (March 31).
For high resolution images of Christine Schmidt and her work, visit /opa/news/00newsreleases/nr_200003/nr_nerve2.html .