AUSTIN, Texas—Viruses associated with the common cold are perfect carriers for DNA, but improvements must be made in the delivery process if the virus is be used in safe and successful gene therapy, says a University of Texas at Austin researcher.
Genetic engineering already permits researchers to use DNA as a sort of drug or therapy vehicle to treat disease. "But direct injection of naked DNA just doesn’t work," said Maria Croyle, assistant professor of pharmaceutics, whose research involves finding a more efficient and safe way for the DNA gene to get where it’s going.
For her research in the development of novel methods of gene delivery, Croyle recently was selected as one of 15 investigators by the American Association of Colleges of Pharmacy to receive grants through its New Investigators Program. The awards assist the research careers of new faculty members within pharmacy colleges and schools in the U.S. and Canada by providing start-up funding for their research.
For some time, scientists have identified missing or altered sequences in chromosomes as contributing factors of many human illnesses including cystic fibrosis, muscular dystrophy, diabetes, cardiovascular disease, cancer and infectious diseases such as hepatitis and AIDS, said Croyle. Once scientists identify the specific gene involved in a particular disorder or illness, gene therapy emerges as a treatment option.
Croyle picked the cold virus or adenovirus because its DNA structure is well known and it can be manipulated. "And, as we know, this virus is good at infecting cells. If we can’t cure the common cold virus right now, let’s at least use it to our advantage," she said.
In her research, Croyle takes the virus DNA out, removing part of the DNA that gives a person a cold. And then she replaces it with the therapeutic gene.
The common cold virus also can be easily produced in large quantities and is capable of producing very high levels of gene expression. (Gene expression is the production of whatever therapeutic gene is put in the virus — if it were for cystic fibrosis then it would be the cystic fibrosis gene.)
“Dr. Croyle’s lab at the university is one of the few academic labs in the country that is dedicated to refining gene therapy vectors or vehicles as viable medicinal products,” said Dr. Steven Leslie, dean of the university’s College of Pharmacy. “She is an emerging leader in this pioneering field and we are thrilled to have her here.”
In the last few years, the importance of safe gene delivery research came to light after severe adverse effects were discovered during clinical trials around the country.
“Enthusiasm for using viruses for gene therapy quickly diminished,” Croyle said. “And, it became apparent that development of an efficient and safe gene delivery system is one of the major challenges in the field of gene therapy.
“Unfortunately, our immune system will attack the virus and get rid of it before it can deliver a second dose of the therapeutic gene material. This is important in the case of the adenovirus as the gene does not stay in the body forever. It is what needs to be corrected if we are going to cure genetic disease.”
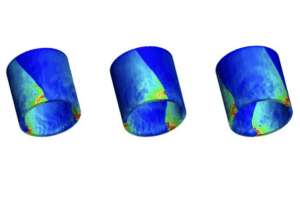
Croyle’s new research involves taking a polymer or liquid plastic and completely covering the virus.
“By doing this we can hopefully reduce the immune response,” she said. “We have learned that this works, but now we need to understand why it’s working before we use it on humans.”
When the problem of immune response against the virus is solved in the lab, Croyle will team up with a clinical scientist to make the improved vehicle into a product.