AUSTIN, Texas—Biomedical engineers at The University of Texas at Austin have received a five-year, $2.3 million grant to investigate an imaging method for detecting the earliest signs of glaucoma so physicians can reduce how often the disease produces vision loss or blindness.
Of the estimated 3 million Americans with glaucoma, half are thought to be unaware they have it because the disease’s subtle progression and painless nature make it difficult to detect.

|
|
H. Grady Rylander III, the physician and biomedical engineering professor who is leading the $2.3 million grant funded by the National Eye Institute to develop an eye exam to detect the earliest stages of glaucoma. At left is a computer monitor image of a “peripapillary birefringence map” used to diagnose glaucoma.
|
| Photo: Patrick Cummings |
Glaucoma results from damage to nerve cells at the back of the eye due to causes that include poor circulation and build-up of fluid in the eye that puts pressure on the ganglion cells. The lack of recognizable symptoms leaves the public reliant on current exams that aren’t as good as possible, often detecting the disease after substantial damage has occurred.
“Glaucoma kills the optic nerve—once it’s gone, we can’t bring vision back,” said H. Grady Rylander III, the physician and biomedical engineering professor who is leading the research.
The researchers will use the National Eye Institute funding to study an imaging machine’s ability to replace current exams. These current exams look for indirect measures of glaucoma—the pressure buildup that occurs 80 percent of the time, or the final loss of vision that results from the ganglion cells dying. The new exam gets directly at the root of the disease: looking for an early sign of ganglion cell death, regardless of the cause of glaucoma.
Rylander, the Harry H. Power Professor in Engineering, and imaging expert Thomas Milner, an associate professor of biomedical engineering, will use a machine to directly visualize inside the ganglion cells where damage occurs that brings on the disease. These nerve cells at the back of the eye carry visual information to the brain, and their gradual loss in glaucoma limits and eventually destroys vision.
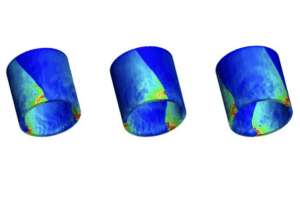
The biomedical engineers will use a device called an Optical Coherence Tomography (OCT) machine to image eye tissue by bouncing light off of it similar to the way ultrasound produces images with sound waves. Traditional OCT machines are used by ophthalmologists to evaluate conditions like macular degeneration that affect the retina.
Rylander, Milner and graduate students in their laboratories will use a modified version of the OCT machine to obtain more detailed information about ganglion cell degeneration in one eye of test animals.

|
|
Thomas Milner, an associate professor of biomedical engineering, provides technological expertise on optical coherence tomography for the glaucoma grant research.
|
| Photo: Patrick Cummings |
The modified OCT machine can measure changes of internal structures within the ganglion cells in greater detail. In particular, the machine can distinguish between normal and damaged cell structures because of the different speed at which light polarized in two directions bounces off the structures. The biomedical engineers will use this capacity to image structural components called microtubules that occur within extensions of the ganglion cells. Microtubules in these isolated extensions called axons are thought to disappear early in glaucoma, perhaps because they are more vulnerable to free radicals there.
“Microtubules are probably one of the first structures that are going to go, and if you could come up with a noninvasive way to measure their disease-related changes, you could come up with ways to protect them from dying,” said Rylander, who sees patients at the Eye Institute of Austin three days a week.
By 2009, Rylander and Mia Markey, an assistant professor of biomedical engineering at the university, expect to begin evaluating 40 patient volunteers at the institute who have glaucoma. The researchers will see how well the data from animals match up with what happens as glaucoma progresses in humans. They will also develop the steps to performing the eye exam in humans.
Within two more years, the OCT protocol will be fine-tuned with 80 patients seen by Dr. Stewart McKinnon, an ophthalmologist and associate professor at Duke University, who runs the university’s glaucoma service. The lead engineers’ ultimate goal is to have the glaucoma exam available for ophthalmologists nationally within 10 years.
“If the test we develop is cheap enough to pursue commercially, and only takes two to three seconds to perform,” Milner said, “it could make a huge difference in reducing how many people lose their vision.”
For more information contact: Becky Rische, College of Engineering, 512-471-7272.