A novel delivery system that could lead to more efficient and more disease-specific vaccines against infectious diseases has been developed by biomedical engineers at The University of Texas at Austin.

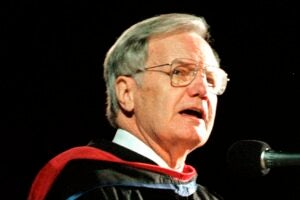
The findings use specific ribonucleic acid (RNA) molecules to significantly bolster a vaccine’s effectiveness while tailoring it based on the type of immune response that is most desirable for a particular disease, says Krishnendu Roy, associate professor of biomedical engineering and lead investigator on the study.
Roy and his team, which included his graduate student Ankur Singh and collaborators at M.D. Anderson Cancer Center in Houston, achieved their results during a two-year study primarily working with a DNA-based hepatitis B vaccine. Their work was recently published in Molecular Therapy, the official journal of the American Society of Gene Therapy.
In their studies using mice, immune responses were five to 50 times stronger than with traditional vaccine delivery. The stronger the immune response to a vaccine, the better protection the vaccinated person should have.
Their research uses a novel polymer-based delivery system that consists of micron-sized particles carrying both the vaccine and the RNA to immune cells.
“What we’ve achieved is a delivery system that provides DNA-based vaccines along with RNA which allows us to significantly enhance the immune response and drive them into a certain direction that is effective against the disease,” Roy says.
The team worked with what are called “silencing RNA,” which shut down specific proteins in the body.
“By silencing certain proteins in the cells that process your vaccine, we can direct the immune response one way or the other,” says Roy, who holds the General Dynamics Endowed Faculty Fellowship.
Physicians want to tailor the immune response because, Singh says, vaccines for parasitic infections may need more of an antibody response, while vaccines for viral infections need more of a cellular response, one that kills the infected cells.
The team’s delivery system would work for a wide range of diseases, making it a broad platform for infectious disease vaccines, Roy says.
Roy says mice studies will continue for the next four to five years. If the tests continue to prove successful, testing could begin on primates and eventually humans within six to 10 years.
“Eventually, we want to try it with (vaccines for) cancer and other auto-immune diseases,” Singh says.
Other collaborators include research fellow Hui Nie and graduate student Bilal Ghosn of the university, and Hong Qin and Dr. Larry W. Kwak of M.D. Anderson Cancer Center.
Funding was provided by the National Institute for Allergy and Infectious Diseases and the Coulter Foundation.
Photos of Roy and Singh are online.