To tell the full story of how his mutant worms may help find better drugs for Parkinson’s disease, The University of Texas at Austin’s Jon Pierce-Shimomura goes back a few decades.

It was the 1970s. Future Nobel Laureate Arvid Carlsson had recently demonstrated that Parkinson’s, which currently afflicts about half a million Americans, resulted from a loss of dopamine-producing cells in the brain. Carlsson, who was a professor at the University of Gothenburg in Sweden, had done his work with mice, which are a good model for testing drugs for humans in terms of their biological similarities. But they are slow. They take awhile to exhibit symptoms, and it takes a lot of time and money for biologically interesting mice to reproduce.
Another future Nobel Prize-winner, John Sulston at the MRC Laboratory of Molecular Biology in Cambridge, England, thought a worm model for Parkinson’s would be cheaper, easier and faster. So he set out to breed a worm with Parkinson’s.
“Sulston and his colleagues found these mutant C. elegans worms that couldn’t make dopamine,” says Pierce-Shimomura, assistant professor of neurobiology at the College of Natural Sciences.
Sulston was on the right track, says Pierce-Shimomura. Biologists have since learned that although humans have a vastly more complex nervous system than the worms, the two species share an “ancient and conserved” genetic structure to their dopaminergic systems. What works to overcome a dopamine deficiency in the worms may also work in humans.
“Nature doesn’t like to give up on a good strategy,” says Karen Mesce, a neuroscience professor at the University of Minnesota. “If there’s a good solution that arises, a biological system that works, then it tends to be maintained, even as species diverge in other ways over millions of years of evolution. Dopamine is a very ancient molecule, and it’s intimately involved in controlling locomotion and motor behavior in humans as well as in simpler organisms like C. elegans, or leeches, or sea slugs.”

The problem for Sulston and his colleagues came when they went looking for symptoms in their dopamine-deficient worms. If they found some that looked like the early symptoms of the disease in humans which include shaking, rigidity and slowness of movement then the worms would be plausible candidates for testing drugs for Parkinson’s.
But the worms, despite their dopamine deficiency, didn’t cooperate.
“As far as he could tell they could crawl and swim fine,” says Pierce-Shimomura. “They didn’t seem to behave like people with Parkinson’s. Sulston was disappointed. He ended up doing fine. He went on to win a Nobel for other work he did on C. elegans, but it’s been a mystery Why can these Parkinsonian worms move so well?”
Over the years the mystery has only deepened as scientists who work with other invertebrates, with similarly stripped down dopaminergic systems, have observed overt Parkinsonian-like symptoms when their organisms are deprived of dopamine.
“If we deprive leeches of dopamine, they become incapable of fluid, harmonious motion,” says Mesce, who works with medicinal leeches. “We observe rigid and jerky motions; they look very Parkinsonian.”
Mystery Solved
Pierce-Shimomura and his graduate and post-doctoral students have now solved the mystery of the Parkinsonian worms. And their sleuth work could lead to up to 1 million potential drugs for Parkinson’s disease treatments being tested on worms each year.

It turns out that the worms do have easily observable Parkinsonian problems. They just need to be given the right set of circumstances in which to exhibit them.
“They can crawl fine,” says Pierce-Shimomura. “They go into a puddle and can swim fine. But as soon as the puddle goes away they crash. In some cases an individual will remain rigid for about a half hour.”
Pierce-Shimomura and his team of researchers, including Andres Vidal-Gadea, Stephen Topper and Layla Young, identified this “motor switching” problem in the course of asking an even more basic science question: Do the worms have two neurobiologically distinct gaits swimming and crawling or are they really just doing the same motion, which happens to look different depending on the environment in which they’re doing it?
It’s been an open question in the field for decades. Through the use of a technique called optogenetics, Pierce-Shimomura and his team have been able to answer it indeed, the worms have two distinct gaits.
The scientists took light-sensitive “switches” from algae and jacked them into the worm’s dopamine neurons. Because the worm’s body is transparent, the scientists were able to shine a light directly through the worm to the modified neurons.

“These molecular switches allow us to turn neurons on with a flash of light,” says Pierce-Shimomura, whose results were published in November in the Proceedings of the National Academy of Science.
“We did that when the animal was in water, and it would immediately switch from swimming to crawling. If you kept the light on for 10 minutes, it would crawl for 10 minutes, and if you switched off the light, it would go back to swimming. It was very convincing.”
While running these experiments they noticed the motor switching problem. When the worm’s dopamine neurons aren’t producing dopamine, they have an extraordinarily hard time making the switch from swimming to crawling. That behavior has a strong correlate in humans with Parkinson’s disease.
“We take these motor transitions for granted,” says Pierce-Shimomura, “like getting up out of a chair or walking through a doorway from one surface to another. But people with Parkinson’s have a terrible time with this. They freeze at the threshold. It looks like we have a very simple worm model for this now.”
Testing More Drugs
The advantages of that model for drug testing are extraordinary.
Time is often a huge barrier to identifying drugs that can prevent or treat diseases such as Parkinson’s. Typically, drugs are tested on mice a process that is expensive and requires one to two years for mice to age while testing just a few dozen drugs at a time.

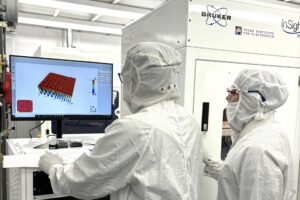
With existing methods, Pierce-Shimomura believes that he can test about 1,000 drugs a year. The number could rise to 1 million a year if the process can be automated.
Pierce-Shimomura and Mechanical Engineering Professor Adela Ben-Yakar recently received a competitive $3 million award from the National Institutes of Health to develop just such an automation process.
To identify potential therapeutics, Pierce-Shimomura begins with worms that have been mutated to be deficient in producing dopamine. The dopamine-deficient worms are put through the same paces that lead to the immobility, but in the presence of a drug.
If they become immobile as they normally would when water is removed, the researchers move on to the next drug. But if somehow a drug helps a worm’s brain overcome the dopamine deficiency and it transitions to crawling, the lab has gained a potential therapeutic.
So far the lab has found one compound that shows promising effects in the worms. The particular compound has already been approved for use in humans for treatment of another condition.
The test is basic enough to run that Pierce-Shimomura has already begun employing undergraduates to do it. He also hopes to employ adults with Down syndrome to run the test (Pierce-Shimomura, whose son has Down syndrome, is very involved in outreach).
“These worms are so simple to work with we can do these drug screens at massive scale,” says Pierce-Shimomura. “Right now the more hands we have, the more targets we can test.”