AUSTIN, Texas — Repurposing drugs such as the FDA-approved niclosamide is a highly efficient way to leverage drugs with known safety profiles to fight the coronavirus outbreak. College of Pharmacy researchers at The University of Texas at Austin are now using new drug delivery formulation technologies to increase niclosamide’s absorption into the body, designing the drug so that it can be inhaled directly into the lungs, which could prove effective at treating and preventing serious COVID-19 virus symptoms in patients.
A collaborative team of researchers in UT Austin’s Division of Molecular Pharmaceutics and Drug Delivery, led by Robert O. (Bill) Williams III and Hugh D. Smyth, is investigating varying methods of drug delivery to repurpose existing drugs into more efficacious forms. The team first focused on niclosamide, recently confirmed to exhibit antiviral efficacy in COVID-19 infected cells. Niclosamide is more potent when compared with other drugs such as chloroquine, lopinavir and remdesivir, and because of its activity as an antiviral drug, it could prove to be an option for treating the virus.
“As soon as we realized the potential health impact of COVID-19, our research teams quickly focused on collaboratively solving the drug delivery problems of niclosamide to allow us to provide additional therapies for physicians to treat this disease,” Smyth said. “The speed at which our team of scientists generated data, found collaborators and planned the pathway to human testing was amazing.”
One problem with using niclosamide as an effective treatment is its poor absorption when taken orally. This limitation of the drug’s properties means that very little, if any, of the drug reaches the target site of the infection. The research team has developed novel drug delivery technologies to overcome these limitations. The team has increased the drug’s apparent solubility and is currently performing oral studies.
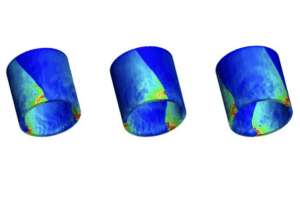
Another approach to overcoming the poor and variable absorption of the drug is to deliver it directly to the infection site. The team, which includes Ashlee D. Brunaugh, Zachary N. Warnken, Chaeho Moon and Miguel Jara Gonzalez, has also developed inhaled forms of niclosamide for protecting and treating respiratory mode of infection, including a micronized crystalline dry powder and an amorphous brittle matrix powder made by thin-film freezing. Since COVID-19 has shown to be particularly damaging to the lungs, delivering an antiviral directly to the site may prove an effective prevention strategy and provide additional treatment options.
“One significant advantage of using an existing drug to treat COVID-19 is it can lessen the time it would take to get it into the hands of doctors and patients,” Williams said. “Outcomes can improve if an existing drug can prove a viable therapeutic option with a new delivery method, lessening the mortality rate and severe medical complications stemming from the virus.”
TFF Pharmaceuticals Inc., which has acquired the patents regarding thin-film freezing and inhalation, is performing an exhaustive exercise reviewing drugs previously approved by the Food and Drug Administration that may be repurposed in an effort to combat the novel coronavirus behind the COVID-19 pandemic outbreak.