The first time I met professor Tom Yankeelov on the campus of The University of Texas at Austin, I was struck by his office’s museum-like walls, covered with photos and paintings from top to bottom. A child’s blue penguin toy immediately caught my attention, spurring a conversation about Yankeelov’s family — the principal creators of all the artwork.
Unbeknownst to me, Yankeelov uses his family’s artistic portfolio as a sort of litmus test for determining the character of whomever enters his office in UT’s Oden Institute for Computational Engineering and Sciences.
Those who talk shop immediately without commenting on the artwork aren’t likely to get an opportunity to work with one of the nation’s most innovative cancer researchers. Being a fan of cute blue penguins turned out to be a serendipitous turn for yours truly.
Kentucky-born to parents from New York and New Jersey, Yankeelov is passionate about many things but none more so than his family and a commitment to using computational science to find new and more effective treatments for patients with breast cancer.
Computational science uses high-performance computing and mathematical models to simulate the behavior of pretty much anything, from weather patterns to the spread of an infectious disease.
Knowing how a tumor will spread could potentially lead to more efficient and targeted therapy, so Yankeelov and his lab have applied this same mathematical modeling approach to breast cancer tumors. In doing so, Yankeelov has dramatically advanced the field of computational oncology since joining UT in 2015 as the W.A. “Tex” Moncrief, Jr. Chair in Computational Engineering and Sciences IV – Computational Oncology and professor of biomedical engineering, diagnostic medicine and oncology.
“Dr. Yankeelov embodies what we mean by ‘change starts here,’” said UT President Jay Hartzell. “He and his colleagues are approaching cancer research in ways that were previously considered radical and ineffective by the medical establishment. Now, his work to apply two seemingly disparate disciplines has put computational oncology on the map and established UT as a societal leader in this area of research that can truly impact the lives of so many people who suffer in some way due to this terrible disease.”
It might come as a surprise that Yankeelov — with a background in physics, mathematics and engineering — is primarily focused on improving outcomes specifically for breast cancer patients.
While in graduate school, he took a seminar on magnetic resonance imaging during an internship at Brookhaven National Laboratory in New York and became interested in using MRI to characterize blood flow in cancer.
Yankeelov continued to delve into imaging methods during his Ph.D. and postdoctoral research, eventually leading him to mathematical modeling of cancer.
This unique combination of mathematical and physics-based expertise and his growing understanding of cancer enabled Yankeelov’s risky decision to reject prevailing medical research methods, choosing instead to explore a fundamentally mathematical approach to cancer.
What if We Had a Mathematical Equation for Cancer?
In a 2019 opinion piece he wrote for The Hill, Yankeelov points to former President John F. Kennedy’s promise that the United States would send a man to the moon within a decade — a promise that was kept and one we continue to celebrate more than half a century later.

By contrast, in 1971 President Richard Nixon proclaimed it was time to attack the growing cancer epidemic with the same enthusiasm and vigor as was applied to the moonshot. More than half a century after the National Cancer Act was signed into law, the disease still has the upper hand.
“Of course, we already had a robust mathematical theory for gravity for almost 300 years at the time of Kennedy’s proposal, but we did not have a mathematical theory for cancer in 1971 — and we still don’t,” Yankeelov wrote.
And without a mathematical theory, he said, we are left with trial and error.
Trial and error remains the predominant method for medical advancements in our treatment and clinical studies of cancer. When a new treatment approach demonstrates efficacy in helping the average person, it is deemed successful despite the likelihood that there may have been several individual patients for whom the treatment was not successful.
In a recent interview with National Geographic, Yankeelov compared prevailing medical scientific research with the approaches taken by aerospace engineers. “When we want to send a satellite into orbit, we don’t launch 100 satellites and hope one of them lands in the right orbit,” he said. “A single satellite is sent to its spot with near perfect accuracy.”
Aerospace engineers are capable of doing this through a heavy reliance on the use of tried and tested mathematical and physics-based principles calculated by the world’s most powerful supercomputers. Fortunately, UT is home to the Texas Advanced Computing Center (TACC), one of the world’s leading academic supercomputer facilities.
Most of the computational research conducted by Yankeelov’s Center for Computational Oncology uses the TACC computing facilities.
While computational science and high-performance computing have had their fair share of critics over the years — pointing toward poor predictive accuracy — the technology has advanced so rapidly in recent times that computer-generated predictions and models have reached unprecedented levels of precision. If their models work for successful rocket launches, then why not for predicting cancer treatment?
The Yankeelov Approach
Yankeelov’s goal is to provide individualized health care by moving beyond “predicting response” to “optimizing response.”
“We try to build mathematical models that make use of individual patient characteristics — not population averages — to predict how a patient’s tumor grows and responds to therapy,” he said.
This, he said, is key to achieving the holy grail of medicine – individualized, patient-centric health care.
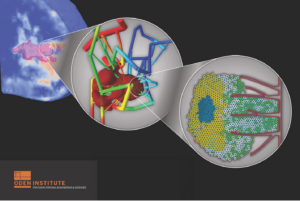
Credit: Chengyue Wu (MDACC), Ernesto Lima (Oden Institute/TACC), David Hormuth (Oden Institute), and Guillermo Lorenzo (Oden Institute).
Aerospace engineering professor and Oden Institute Director Karen Willcox said Yankeelov is at the forefront of developing oncological digital twins that are transforming cancer treatment.
As the name suggests, digital twins are a digital representation of a physical object, person, process or system that allows scientists and engineers to simulate real situations and their outcomes, ultimately allowing them to make better response decisions.
“Tom is a visionary in developing a computational science pipeline that integrates physics-based tumor modeling with patient data to drive treatment decisions, and, importantly, he recognizes the critical role of clinical collaborations to ensure impact,” Willcox said.
AI and Big Data – Big Panacea or Misguided Medicine?
Many cancer researchers getting the most attention right now are working in artificial intelligence and big data. Much stock is being placed in the idea that combining new AI technologies with as much patient-specific data as possible offers the best chance we have at making a breakthrough in cancer treatments.
Yankeelov, who holds positions in UT’s Dell Medical School and the Department of Biomedical Engineering in the Cockrell School of Engineering, has never subscribed to this thesis, and has, in fact, been very vocal about its shortcomings.
“I fear a trap we have fallen into is our commitment to the philosophy of big data and machine learning in attacking cancer,” Yankeelov said. “The belief is that if we collect enough data on enough patients, then we will be able to find statistical patterns indicating the best way to treat patients and find cures.”
While acknowledging that there is certainly a place for the methods of artificial intelligence in medicine, he does posit that the “machine-learning-only” approach is fundamentally misguided. This isn’t simply Yankeelov’s opinion. There are some high-profile cases where AI and big data methods have proved unsuccessful.
“Machine learning relies on properties of large groups of people that hide characteristics of the individual patient. This is especially problematic for a disease that manifests itself so differently from person to person,” Yankeelov said. “Indeed, cancer is not even one disease; there are dozens of cancers.”
Bringing Together the Best Collaborators
One of Yankeelov’s other key strengths — aside from his unique expertise and foresight to use mathematical frameworks to address cancer in the same way the fundamental principles of physics and mathematics played central roles in NASA reaching the moon — is his incredible capacity to bring together faculty members from distinct disciplines and create a collaborative environment that allows for real innovation to emerge.
The role he has played in establishing a partnership with MD Anderson Cancer Center — a fellow UT institution that ranks No. 1 in the nation for cancer care — is perhaps the most high-profile example of his strength in bringing people together.
A few years ago, Yankeelov and John Hazle, a medical physicist and chair of MD Anderson’s Department of Imaging Physics, Division of Diagnostic Imaging, started thinking about formalizing the growing partnerships between their groups in computational oncology.
With the support of Willcox of the Oden Institute, Dan Stanzione of TACC and David Jaffray of MD Anderson, Yankeelov and Hazle this year established the Center for Computational Oncology — a partnership between the Oden Institute, TACC and MD Anderson.
“Tom’s enthusiasm and diligent drive to bring these unique talents and resources together was a major factor in the successful launch of the CCO,” Hazle said. “Tom is an outstanding collaborator.”
In the short time since the organizations began collaborating, dozens of faculty members and researchers have already published papers with significant findings in key areas.
One study looked at how integrating MRI data with biologically based mathematical modeling could successfully predict breast cancer response to chemotherapy. The findings suggest digital twins could facilitate a paradigm shift from simply assessing response to predicting and optimizing therapeutic efficacy.
Another key collaboration found that gliomas, which can be extremely difficult-to-treat brain tumors, have greater resilience, therefore requiring more trial-and-error chemotherapy. This discovery led to a new technique that would use noninvasive imaging approaches that can measure a tumor’s properties, which can then be used to calibrate patient-specific mathematical models of tumor growth and response.
“These examples illustrate how we’re working to eliminate the trial-and-error approach to cancer treatment,” Yankeelov said. “We don’t tackle other types of scientific research with the inherent uncertainty that comes with trial and error. Why would we approach health care in this way?”